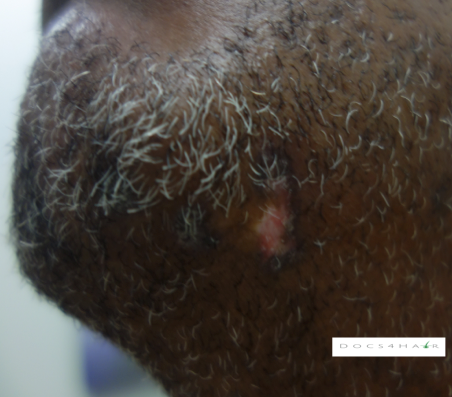
Discoid lupus
Clinical Presentation (1, 2)
Discoid lupus erythematosus (DLE) is a progressive primary lymphocytic scarring alopecia (initial lesions may be non-scarring). It is classified as a type of chronic cutaneous (skin) lupus erythematosus. A fully evolved lesion presents with sharply-demarcated red, scaly plaques with a central depressed scar, central skin lightening, follicle scale plug, and a surrounding dark patch (3). It can occur on the face, ears and scalp, and upper body (rarely in the mouth and genitals). Up to 60% of DLE sufferers have scalp involvement. It can be associated with itching or pain, although some people have no symptoms.
Epidemiology (2, 4)
DLE is more common among black females. It occurs 4-5 times more common in black women compared to white women (2, 4), Black women tend to present earlier and die earlier when compared to whites (McDaniel 2018). The typical age of presentation is between 30 and 59 years of age (1, 2, 4)
Causes (2)
DLE is an autoimmune condition characterized by a loss of immune tolerance/ privilege
Diagnosis (1)
DLE is diagnosed via careful history, clinical scalp and hair exam, and dermoscopic evaluation (5, 6). Scalp biopsies may be performed to help confirm the diagnosis.
Clinical Imitators (Differential Diagnosis) (1, 2)
Lichen planopilaris, frontal fibrosing alopecia, Graham–Little syndrome, alopecia areata
Associated Conditions
Systemic: Systemic lupus erythematosus (SLE) may develop in 5-25% of people with DLE (7, 8, 9). The risk for SLE is increased when DLE lesions are found below the head and neck, nail changes (periungual telangiectasias), joint pain, and high levels of lupus screening test antibody (ANA) are observed. The mean time to progression of SLE is approximately 8 years.
Skin: Squamous cell skin cancer (SCC) may develop in long standing DLE lesions (10, 11). A 4-fold increase in the risk of SCC has been reported in people with DLE (11, 12).
Treatment (1, 13, 14)
Early recognition is key to management. The goal is to halt/ stabilize the spread of disease and to relieve signs and symptoms. Hair regrowth is NOT possible after the follicles are replaced by scar tissue.
Prevention: Strict sun protection, stop smoking (2))
Active DLE:
Anti-Inflammatory: Oral antimalarials (hydroxychloroquine) (Milam EC), topical calcineurin inhibitors (tacrolimus- topically compounded at higher dose) and pimecrolimus) (15), steroids (topical/ injection), oral tetracyclines (tetracycline, minocycline, doxycycline), other oral/ injection immunosuppressives (methotrexate, dapsone, thalidomide, mycophenolate mofetil, rituximab/ ustekinumab/ intravenous immunoglobulin (severe disease)),
Retinoids: Topical and systemic
Other emerging: Pulse dye laser (16)
End stage CCCA: Irreversibly scarred areas of baldness, despite treatment
Scalp camouflage: Hair fibers, color stick, and scalp prosthesis (e.g.. customized wigs)