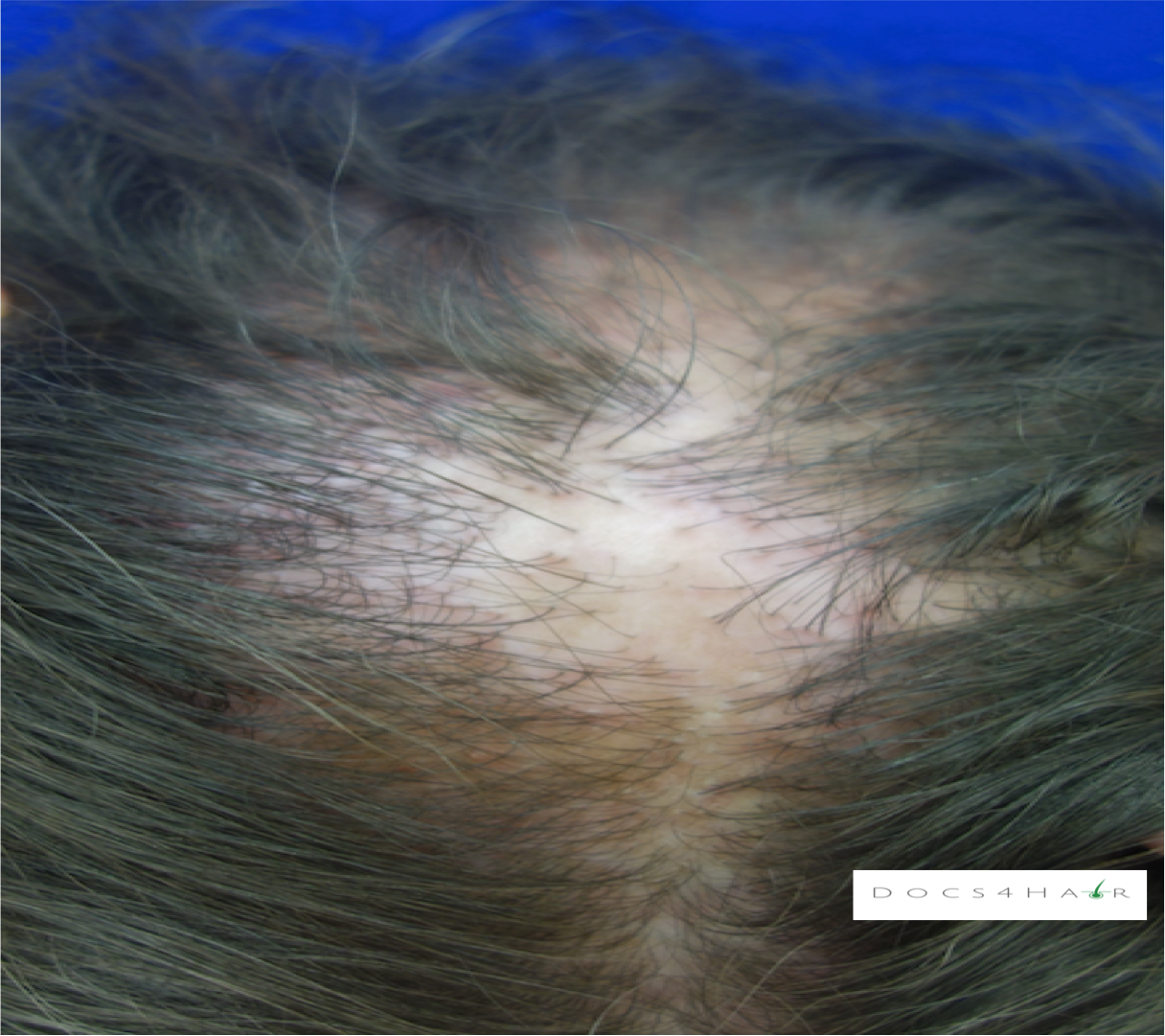
Lichen Planopilaris
Clinical Presentation (1, 2, 3)
Lichen Planopilaris (LPP) is a chronic progressive primary lymphocyctic scarring alopecia. It presents with red rough bumps/pimples around the follicle and patchy thinning/ balding. It may also be associated with itching, burning, pain, and hair shedding. There are two clinical types (frontal fibrosing alopecia, and Graham-Little Syndrome).
Epidemiology (1, 2, 3)
The typical age of onset of LPP is between 30-60 years. Although it can affect men and women of all ethnicities, it is more common in Caucasian women.
Causes (4, 5)
The exact cause of LPP is unknown. However, some proposed mechanisms include autoimmune dysfunction (follicle immune cell privilege collapse), reduction in peroxisome proliferator-activated receptor gamma (PPAR-γ or PPARG), genetic predisposition, and more recently interferon (IFN)-γ dysfunction.
Diagnosis (6, 7)
LPP is diagnosed via careful history, clinical scalp and hair exam, and dermoscopic evaluation. Scalp biopsies may be performed to help confirm the diagnosis.
Clinical Imitators (Differential Diagnosis) (3)
Alopecia areata, Central centrifugal cicatricial alopecia, discoid lupus erythematous, frontal fibrosing alopecia , folliculitis decalvans, female pattern hair loss, and traction alopecia.
Associated conditions (5, 8)
Thyroid disease, hirsutism.
Treatment Options (9)
Early recognition is key to management. The goal is to halt/ stabilize the spread of disease and to relieve signs and symptoms. Hair regrowth is NOT possible after the follicles are replaced by scar tissue.
Active LPP: Red scaly bumps around the hair follicle associated with hair loss, stinging, burning:
Anti-Inflammatory: Oral antimalarials (hydroxychlroquine), steroids (systemic, topical/ injection), oral immunosuppressives (methotrexate, mycophenolate mofetil, cyclosporine), oral tetracyclines (tetracyline, minocycline, doxycycline), topical calcineurin inhibitors (tacrolimus and pimecrolimus),
PPAR-γ modulators: Pioglitazone
Growth stimulants: Minoxidil (anagen phase promoter- topical)
Other therapies: Excimer laser (10), low level light therapy (11), low dose naltrexone (12),
New emerging (13): Janus kinase inhibitors (Tofacitinib )
Hair Restoration (14, 15, 16): Platelet rich plasma
Hair grooming: Avoid potentially damaging hair care practices such as traction/ tension hairstyles (weaves, wigs, braids, extensions, ponytails, etc.), chemical relaxers, excessive heat, hair bleaching, and hardening gels and sprays. The aforementioned practices may further compromise an already fragile hair and increase breakage. Follow-up with a hair care professional who is well versed on safe hair care practices.
End stage LPP: Irreversible scarred shiny areas of baldness, despite treatment
Scalp camouflage: Scalp micro-pigmentation, hair fibers, color stick, and scalp prosthesis (e.g customized wigs)..
Hair transplantation: Extreme caution should be exercised due to the possibility of disease reactivation and decreased efficacy (17). Test grafts of 50-100 hair follicle units may be transplanted into non-active areas and monitored for a year before larger surgeries are attempted (18). If transplants are performed, at least 1 year of medical therapy and at least 2 years of remission/ stabilization of disease with no symptoms (redness, itching, pain, hair loss, etc.) off medications is preferred (18). Medication use after hair transplants is encouraged but is done at the discretion of the medical and surgical team.